Physician Leadership and Engagement: A Critical Priority for Healthcare
Introduction: Leading in a “BANI” World
Over the last 30 years, strategists, consultants, and business leaders have frequently spoken of operating in a VUCA (Volatile, Uncertain, Complex, Ambiguous) world. Despite its prevalence, this structure no longer fully captures the intensity and unpredictability healthcare leaders face today.
Enter the BANI framework, a new paradigm coined by Jamais Cascio. As a forecaster for the California-based think tank Institute for the Future, Cascio realized that global institutions and systems were becoming much less durable than they had historically been. BANI—which stands for Brittle, Anxious, Non-Linear, and Incomprehensible—elegantly captured the burgeoning chaos that has come to define the modern context.
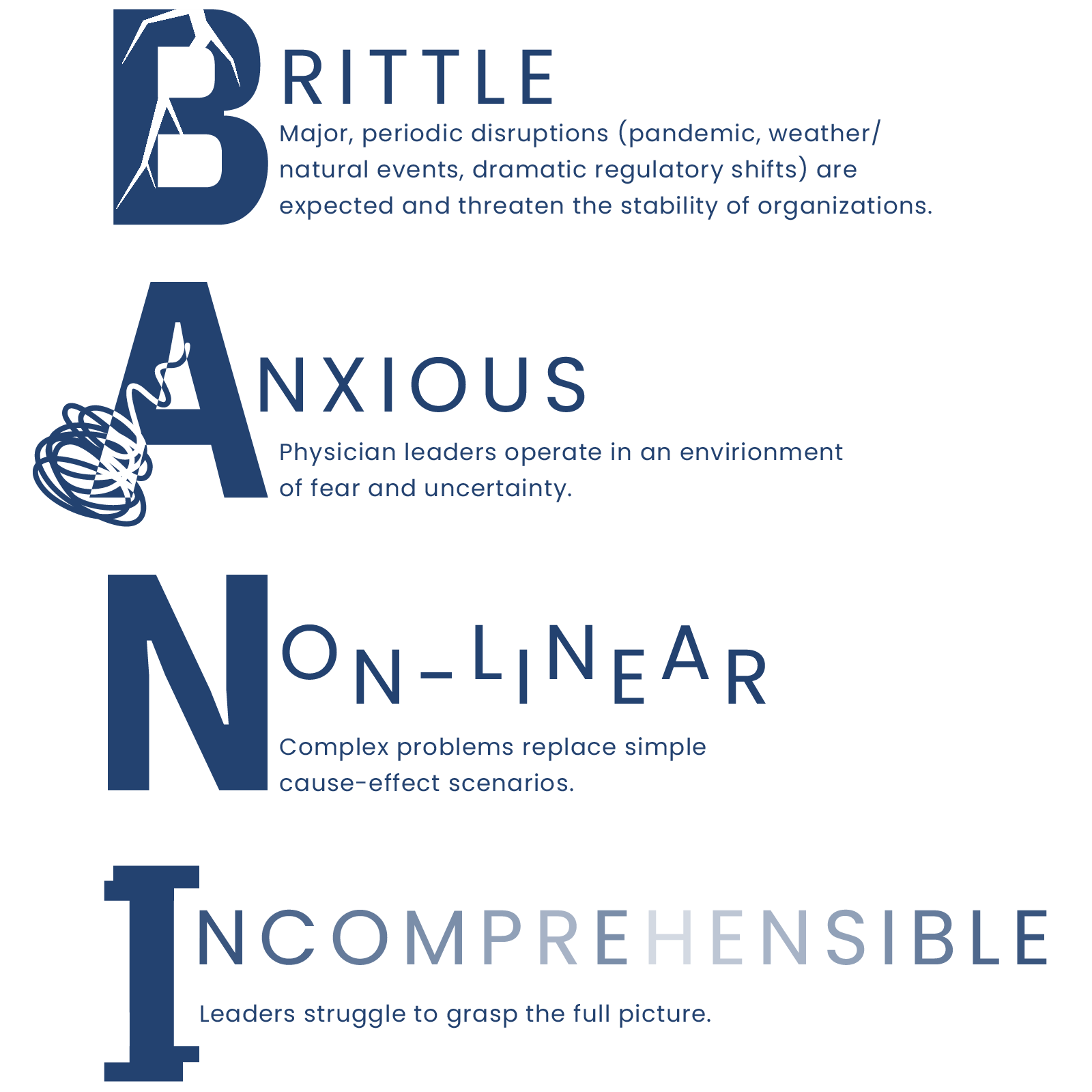
No domain reflects our BANI context like American healthcare, marked by unpredictable crises like the COVID-19 pandemic, climate change and related weather events, and shifting regulatory demands. What has seemed stable can shatter unexpectedly (Brittle), leaving physicians and healthcare workers grappling with anxiety and fear about the future (Anxious). The U.S. healthcare industry has become so complex that simple cause-and-effect relationships no longer apply (Non-Linear), and the overwhelming flow of information makes it increasingly difficult to grasp the full picture (Incomprehensible).
As Cascio notes, the antidote to BANI problems is rooted in deeply human approaches that leverage resilience, empathy, improvisation, and intuition. This has substantial implications for healthcare leaders, who must help organizations navigate deep, sudden shifts that ripple through the U.S. healthcare industry. In this article, we explore how healthcare leaders can apply these insights to engage physicians more effectively and why investing in physician leadership development is crucial for navigating the chaos of the BANI world.
The Case for Change: Physician Engagement in a Brittle System
The BANI framework reveals deeper cracks within our hospital and health systems, making a strong case for reevaluating how we engage physicians in leadership roles. For example, the brittle nature of the system means that the sudden breakdowns we’ve witnessed—such as hospitals overwhelmed during a pandemic—are not just isolated incidents but indicators of a deeper fragility. At a point in time where minor disturbances can have far-reaching consequences, traditional physician engagement strategies—which tend to keep clinicians at a distance, serving more as advisors rather than decision-makers—are no longer sufficient.
Physicians feel the strain of this brittleness. The fine line between clinical and administrative decisions has nearly dissolved, making patient care increasingly dependent on factors they feel are outside their control. The anxiety that comes with navigating such a volatile environment can leave physicians feeling powerless, contributing to disengagement and a reluctance to step up to executive roles. In a world where outcomes are increasingly non-linear—where seemingly small decisions or changes can have massive, unpredictable consequences—hospital & health systems need their medical staff to feel equipped and supported by their organizations to handle complexity. But instead, they are frequently overwhelmed by the sheer incomprehensibility of the structure they operate within.
Unsurprisingly, an outcome of this BANI environment is increased frustration (at best) and burnout (at worst) among physicians. The COVID-19 pandemic exacerbated these issues, with many physicians struggling to balance patient care with their own mental health and well-being. The situation is particularly dire for mid-career physicians, who are caught between clinical duties and other responsibilities. A 2024 survey by CompHealth revealed that many physicians feel they lack adequate support and resources to thrive in their roles.
At the heart of the physician engagement problem is the hazy-but-enduring cultural dichotomy between clinical practice and healthcare administration. Physicians are likely to feel called to the former and ambivalent (if not actively hostile) to the latter. Sidelined in decision-making processes led by non-clinical administrators, physicians may recognize the opportunity to have greater influence as executives but are unlikely to be incentivized to do so. This disconnect fuels frustration and disengagement, contributing to higher burnout rates and lower job satisfaction.
Addressing these challenges requires a systemic shift in physician leadership development—one that recognizes and reinforces the fact that all physicians lead. The impact and reach that physicians have puts them in informal leadership roles, despite a lack of formal leadership training; moving them into more formal leadership roles could turn the negative tide created by BANI. This requires action.
To develop a deep bench of physician leaders, hospital & health systems must genuinely recognize the value that clinically trained executives can contribute to their organization and establish appropriate incentives and support to encourage and develop them. Formal leadership development programs that provide coaching, skill development, and peer learning are an essential piece of this work.
What we’ve found most impactful in developing physician executives is providing them with the opportunity to re-imagine what they can contribute to their organizations as leaders. Ideally, this occurs as members of a developmental cohort, where participants become part of a diverse learning community of practice focused on hands-on learning, relevant experimentation, and structured reflection with trusted mentors and coaches.
Cohort development works best when physicians can expand their thinking about leadership by hearing external perspectives. This should then be put into action by applying learnings within the organization: this enables physicians to contribute to high-level decision-making and organizational strategy, which in turn builds understanding and increases engagement. Development should also provide opportunities to address the unique challenges mid-career physicians face, offering them the support they need to thrive as leaders while continuing to deliver high-quality patient care. Throughout, a focus on self-management is required to reflect the importance of physician mental health and well-being, helping physicians build resilience and manage the stresses of leadership.
By focusing on both professional and personal development, this approach helps physicians embrace the challenge and opportunity of administrative roles, enabling them to have greater impact on patient outcomes and become leaders who are better equipped to navigate the challenges of modern healthcare.
As hospitals continue to face unprecedented challenges, now is the time to invest in physician leadership and ensure that clinicians are not just surviving but thriving in their roles. By investing in leadership development, health systems can create a more engaged, resilient physician workforce—one that is not only prepared for today’s challenges but also for the unpredictable shocks of tomorrow.
Capable, resilient, and empathetic physician leadership is not an option—it is a necessity. The health and success of our health systems depend on it.
References
- CompHealth. Physician salary 2024: Incomes increase, but many are unsatisfied
- James Cascio. Human Responses to a BANI World
- The Physicians Foundation: New Survey Uncovers the Future of Medicine is in Jeopardy
- WU Executive Academy. BANI vs. VUCA: How Leadership Works in the World of Tomorrow











