The Multifaceted Role of CHROs in US Healthcare Delivery
CHROs in a Changing Healthcare Landscape
The role of Chief Human Resources Officers and Chief People Officers (CHROs) is becoming increasingly complex and challenging, expanding the scope of human resources (HR) to encompass a broader spectrum of roles, functions, operations, and technologies. In fact, a significant majority of HR teams (83%) now take on more responsibilities compared to three years ago, handling an increasing variety of requests and topics (55%) and facing different challenges than those they faced pre-pandemic (80%) (Gartner, 2023). Given the shift in business demands and models of work, HR functions must adapt and transform accordingly to stay responsive and effective. Currently, only 9% of HR teams are both highly efficient and highly aligned with their organizations’ needs (Gartner, 2023), suggesting that there may be opportunities to enhance HR’s impact and alignment with the business.
CHROs in healthcare play a critical role in building a people-centric culture that is essential for delivering high-quality patient care and prioritizing the wellbeing of healthcare professionals. At the same time, healthcare CHROs face unique challenges beyond those in other industries, including talent shortages and safety concerns that contribute to greater stress and burnout among healthcare professionals (CDC, 2023). In this context, HR leaders need to navigate how to increase efficiency without overburdening teammates and decreasing quality of care. They must balance the need to implement change with the importance of maintaining a supportive and respectful work environment while building a talent bench for the future. This requires a deep understanding of the unique challenges facing healthcare professionals, as well as the ability to develop and implement strategies that address these challenges.

To succeed in this dynamic healthcare landscape, CHROs need to evolve and transform HR’s role within their organizations to meet business and talent needs in a sustainable way. Drawing on our extensive history of partnering with healthcare organizations and leveraging our proprietary research about the evolution of the healthcare CHRO role, we provide comprehensive insights into the contemporary CHRO mandate, the factors leading to success, and actionable recommendations for how CHROs can succeed in the face of change.
Factors Impacting the Evolution of the CHRO Role in Healthcare
Several key trends and challenges are shaping the rapidly evolving role of HR in healthcare and the mandate and responsibilities of CHROs.
Economic Pressures
Economic fluctuations, rising healthcare costs in areas like labor, pharmaceuticals, and supplies, and a growing administrative burden put immense pressure on healthcare budgets. This financial strain challenges healthcare providers’ ability to maintain their commitment to delivering 24/7 care for the patients and communities they serve (AHA, 2024) and causes financial performance margins to lag behind pre-pandemic levels (McKinsey, 2024a). Despite a stable outlook for nonprofit hospitals in 2025, the recovery remains uneven and incomplete as challenges persist, including the labor market, payer environment, antitrust enforcement, and new administration policies (Kaufman Hall, 2024). As healthcare providers adapt to a new normal, they continue to face a long and arduous journey ahead.
Technological Advancements
Technological shifts such as digital technologies, telehealth, and artificial intelligence (AI) are poised to transform the way healthcare is delivered, experienced, and managed. AI tools, in particular, can contribute to enhanced operational efficiency in administrative tasks and improved patient experiences from pre-care to long-term follow-ups (Forbes, 2025), generating between $60 billion and $120 billion of potential savings for hospitals within the next five years (Healthcare Dive, 2023). In medical sciences, AI revolutionizes treatment and delivery, with early advancements in diagnosis and image analysis, robot-assisted surgery, and virtual nursing assistance, among other use cases. These technological advancements support more cost-effective, equitable, and innovative healthcare delivery, while decreasing unnecessary hospital visits and enhancing patient care.
Organizational Transformations
The healthcare industry has been undergoing significant and rapid changes since 2020, with many organizations undergoing structural shifts such as mergers, acquisitions, and portfolio realignment, as well as operational adjustments, workforce restructuring, and the development of new business models. Besides the high volume of announced M&A transactions in 2024, a more concerning message lies beneath: the percentage of transactions involving a financially distressed party and the percentage of transactions involving a divestiture both reached record highs (Kaufman Hall, 2025). The volatility and accelerated pace of change resulting from disruptions can threaten healthy organizational culture, a critical factor for value creation, resilience, and safety in the healthcare sector (McKinsey, 2024b). Furthermore, the constant state of flux can lead to change fatigue among healthcare professionals, further deteriorating burnout and disengagement.
Skilled Talent Shortages
The scarcity of skilled talent in healthcare is a pressing concern, with the shortage of nursing staff, physicians, and other frontline healthcare professionals reaching critical levels. Although the talent shortage shows signs of stabilization compared to the years of the COVID-19 pandemic, projections suggest continued strains. By 2028, the US is anticipated to have a national shortage of 100,000 healthcare professionals, with some states projected to have surpluses and others with deficits of up to 14,000 (Advisory Board, 2024). Recent data indicates that 20% of hospital workers vacated their positions in 2023, with 47% contemplating leaving their current roles within the next two years (Definitive Healthcare, 2023). Critically, turnover among nursing staff, who are pivotal to maintaining high standards of patient care, persisted at a significant rate of 18% (Becker’s Hospital Review, 2024).
Wellbeing and Safety
Healthcare professionals’ wellbeing, across ranks and functional areas, is suffering. Healthcare team members face demanding and sometimes dangerous duties, including exposure to infectious diseases and violence from patients and their families. According to a CDC Worklife survey comparing professionals across industries, healthcare professionals are more likely to report poor working conditions and poor mental health days than their peers in other industries. Furthermore, the number of healthcare teammates reporting harassment at work doubled from 2018 to 2022 (CDC, 2023). Despite some improvements, physician burnout remains a serious issue, with nearly 45% of physicians experiencing burnout in the first half of 2024 (AMA, 2024). In conjunction with current social, political, and cultural forces, CHROs need to consider new ways to strategically drive greater safety. This includes implementing safety measures and developing initiatives, protocols, and routines throughout the organization that create a supportive environment with physical and psychological safety.
The Evolution of Healthcare CHROs: A Modern Leadership Portrait
The role of healthcare CHROs has traditionally been primarily focused on areas such as employment policies and administration, where HR served as the main manager of these responsibilities. However, as healthcare organizations face new driving forces, the CHRO role becomes increasingly complex and interconnected. To thrive in this new environment and help achieve organizational success, CHROs need to drive functional excellence while also transforming into a “strategic connector” within the organization.
To further understand these trends and their importance, WittKieffer conducted a comprehensive analysis examining both the backgrounds and career paths of today’s CHROs at leading health systems, as well as the evolution of leadership profiles from pre-pandemic to present.
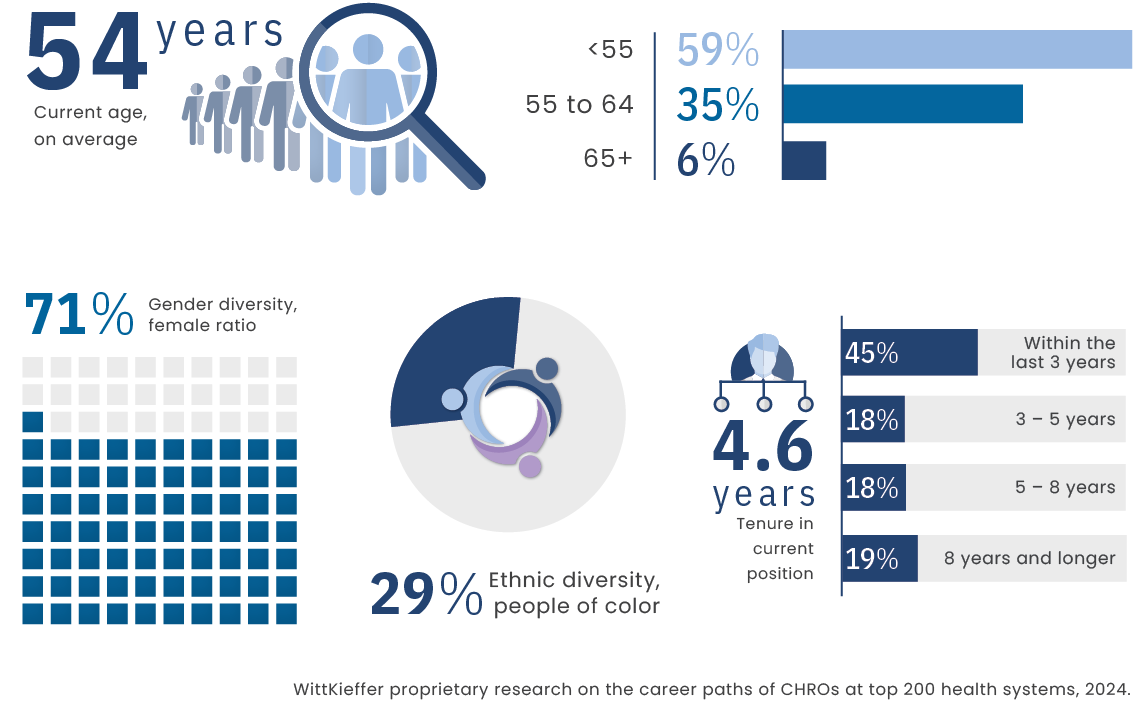
Pathways to the Top HR Role
Today’s healthcare CHROs represent a compelling story of diversity and transformation in leadership. The educational backgrounds of current healthcare HR leaders reflect their sophistication, with MBAs (25%) and MS degrees in HR/Labor Relations (20%) being the most common. JDs follow closely behind, making up 11% of the field. Most CHROs in health systems are female (71%), and more than one in four are people of color (29%), showcasing significant advancements in leadership variety. The average CHRO is 54 years old, and the age spectrum spans remarkably from 35 to 71 years, bringing together multiple generations of leadership perspectives.
What is particularly striking is recent turnover: nearly half (46%) of current CHROs have stepped into their roles within the last three years, compared to 30% among CEOs at the same health systems. This signals a significant leadership refresh across the healthcare HR function and suggests that the industry is actively reshaping its HR leadership to address existing and emerging challenges.
A Demographic Profile of Health System CHROs
From Entry Level to C-Suite: A Look at Health System CHRO Career Paths
While more than one in four (28%) have built their entire careers within healthcare, many bring cross-industry experience from professional services (such as law, consulting, and HR/staffing; 19%) and consumer/retail sectors (17%). By the time they reached the position before their current CHRO role, the vast majority (91%) had transitioned to healthcare, with most (85%) serving in a hospital or health system setting.
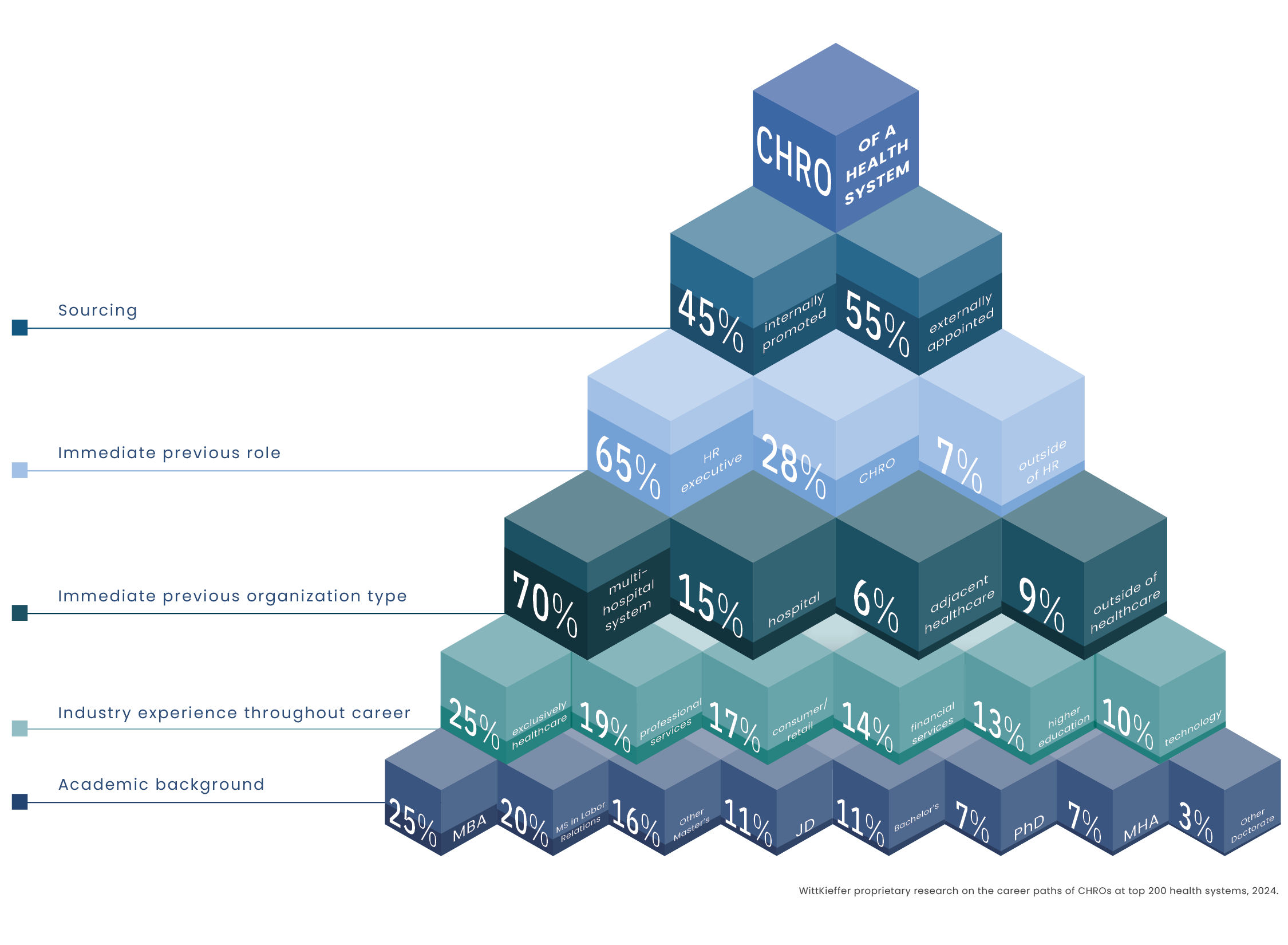
Career Pathways to the CHRO Position Reveal Four Distinct Profiles:
INTERNAL “STEP-UPS”
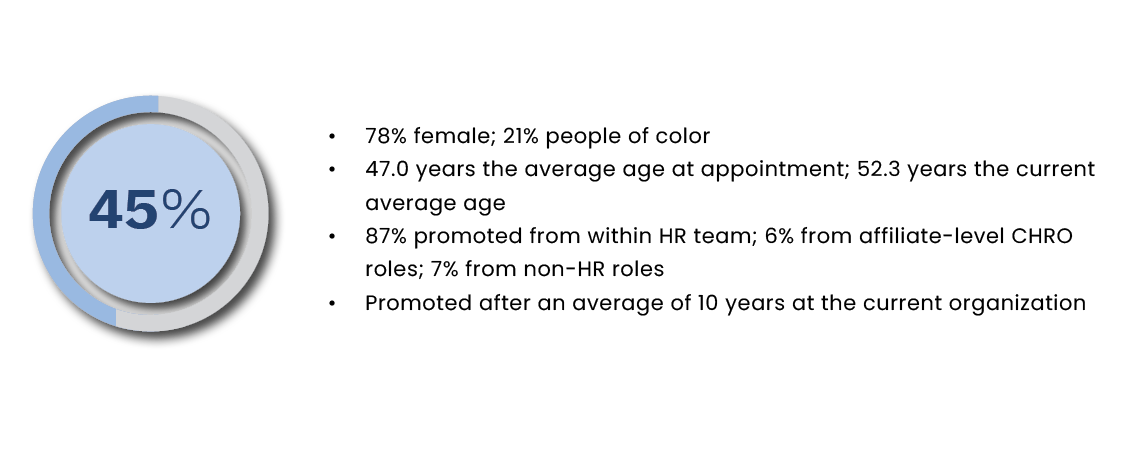
These HR leaders, who advanced through the ranks of their organizations before reaching the top HR position, skew more heavily female than other profiles. On average, they assumed the CHRO role at age 47, following approximately 10 years of service within their organizations. Notably, larger systems draw from their deep internal leadership bench, while smaller systems rely more on external talent. Specifically, 69% of CHROs at large systems (those with revenue of $10 billion or more) have been promoted from within, compared to 44% at medium-sized systems (revenue of $2 to $10 billion) and 37% at small systems (revenue less than $2 billion).
EXTERNAL “STEP-UPS”
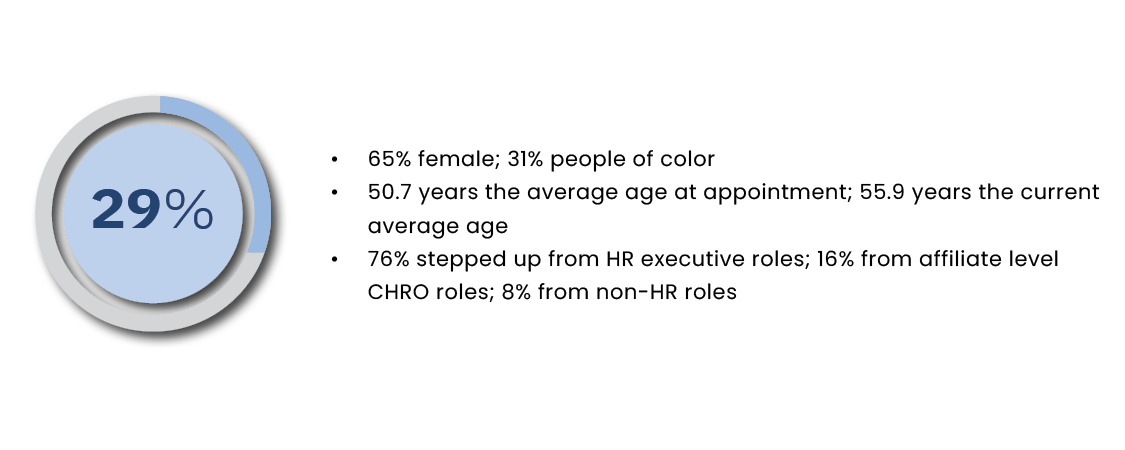
This group assumed their roles at a slightly higher average age (50.7 years). While their career progression mirrors that of internal “step-ups,” these executives ultimately secured their first CHRO position by moving to a new organization.
SITTING SYSTEM CHROs
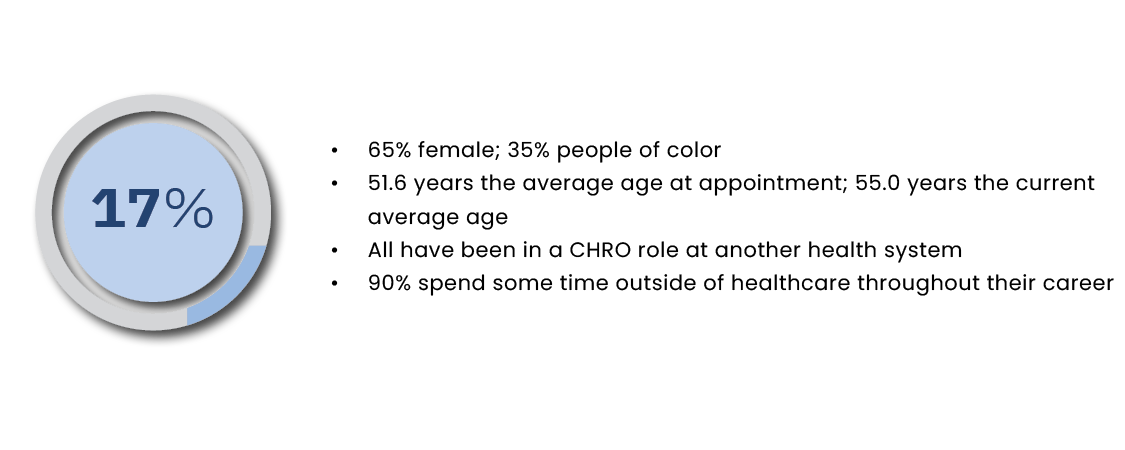
Their higher average age at appointment (51.6 years) reflects their prior experience in system CHRO roles. Remarkably, the vast majority (90%) of these leaders gained experience outside the healthcare sector during their careers.
INDUSTRY SWITCHERS
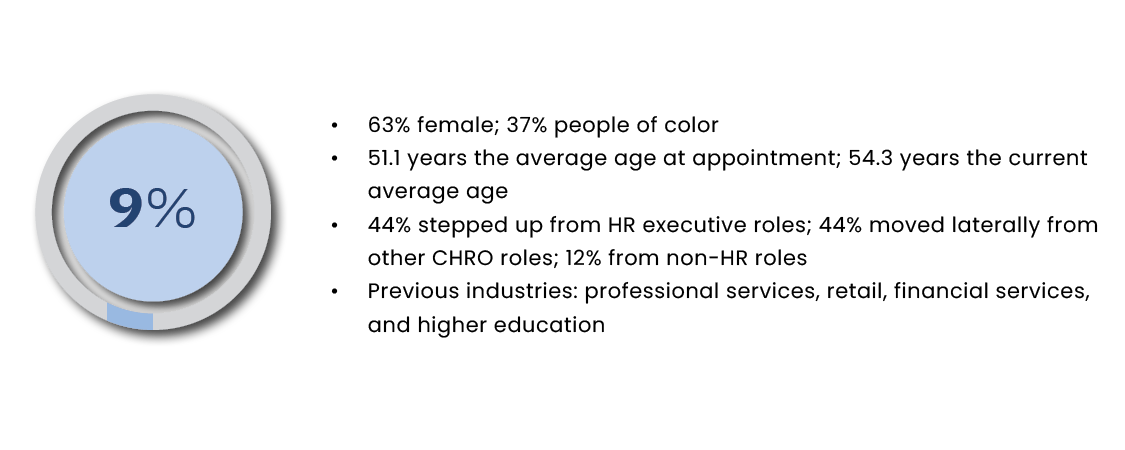
These HR leaders entered healthcare from diverse sectors, including professional services, retail, financial services, and higher education. Their previous experience is evenly split between former CHRO roles (44%) and functional/regional HR leadership positions (44%). The remaining portion (12%) came from non-HR roles, though most brought significant HR experience from earlier in their careers or from HR-adjacent functions. Though many organizations recognize the value of cross-industry perspectives in healthcare HR leadership, successfully transitioning into this highly regulated sector remains challenging. The proportion of current healthcare CHROs from other industries (9%) falls below the cross-industry average seen in S&P 250 companies (28%).
The Extended Mandate of CHROs
Our qualitative analysis of health system CHRO leadership profiles from pre-pandemic to present reveals a significant elevation of the role. Today, 9 out of 10 health system CHROs report directly to the CEO, positioning them to seamlessly integrate with executive leadership and effectively translate organizational vision into strategic talent initiatives.
Today’s CHROs typically oversee teams of 5-7 direct reports — and while HR team structures maintain relative stability, the evolution of CHRO direct reports’ titles reflects a fundamental shift in how healthcare organizations approach talent management. More specifically, a notable transformation is evident in the transition to more comprehensive and expertise-driven role designations. For example, “compensation” is evolving into “total rewards,” and general HR leadership roles are being replaced by specialized functions such as organizational development, talent management, and talent acquisition. These title modifications signify more than mere nomenclature changes; they represent healthcare organizations’ strategic shift toward integrated, people-centric HR approaches.
In response to changes and external forces in the dynamic healthcare market, the role of CHROs has expanded beyond traditional HR responsibilities, primarily focused on compliance and administration. CHROs are now increasingly focused on building and maintaining a diverse and future-ready workforce. Recent leadership profiles highlight the importance of CHROs collaborating with senior leadership to create innovative talent solutions that address critical skill gaps and position organizations for success.
The following areas of impact emerge as additional priorities in contemporary CHRO mandates:
Strategic Transformation and Change Management
CHROs lead strategic initiatives, ensuring the healthcare organization remains agile and responsive to change. Acting as strategic partners to senior leadership, CHROs influence decision-making and align HR strategies with business objectives.
Workforce Development and Talent Management
Developing strategies to attract, retain, and develop top talent is a critical focus for CHROs. Succession planning is equally prominent, requiring CHROs to ensure succession plans are in place for key roles to maintain leadership continuity.
Board Engagement and Strategic Advisory
CHROs serve as strategic advisors to the board and the CEO, using their HR expertise to influence and contribute to high-level decisions. CHROs are required to establish strong relationships with the board and senior leadership through transparency and trust.
Cultural Transformation
CHROs are responsible for fostering an environment that is safe and respectful, where individual uniqueness is celebrated and where the organization’s code of behavior is amplified by its workforce. Enabling cultural transformations that align with organizational goals and values, with patient centricity at the core, is a key focus for CHROs.
Technology and innovation CHROs drive technology integration initiatives to streamline HR operations and enhance employee experience. They are required to utilize data analytics to provide insights into HR metrics and empower data-driven decision-making.
Key Facets of Successful Healthcare CHROs
Changing demands and novel challenges require CHROs in healthcare to be adaptable, forward-thinking, and strategic in their approach to managing human capital. Based on our experience in attracting and partnering with healthcare CHROs, we propose a model for CHRO leadership that consists of five key facets. These facets align with and expand upon Ulrich’s HR model (HRM, 1995), which outlines how HR can evolve from a function-oriented to a partnership-oriented approach.
These facets of leadership are contextual and may have different levels of importance depending on the healthcare organization’s overall strategy and current CHRO leadership imperative. Successful CHROs bring expertise and skills in each area and can leverage them as needed to meet their organizations’ unique challenges and opportunities at a given time.
The “Diamond” Model of CHRO Leadership
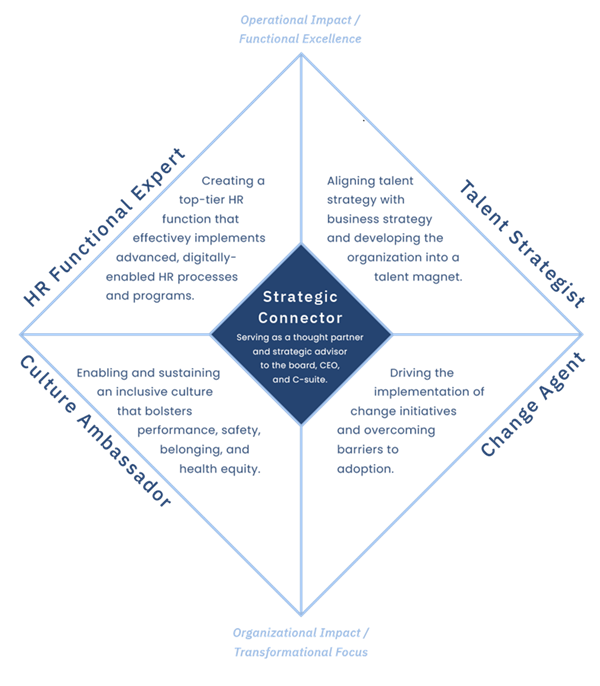
HR Functional Expert
The CHRO role remains indispensable to driving and sustaining excellence of HR functions that serve as cornerstones of organizational success. CHROs lead day-to-day operations of functional areas, including talent acquisition, total rewards, compliance, employee relations, performance management, and learning and development. Functional excellence requires healthcare CHROs to be proactive in developing future-focused approaches to HR functions that are responsive to shifts and keep pace with new human capital demands. In today’s environment, it also includes championing tech-driven transformation in leveraging technology to streamline HR processes and enhance employee experience, including the use of AI for talent acquisition, data analytics for strategic talent planning, virtual reality for training and development, and more.
Talent Strategist
From initial talent attraction through career advancement to succession planning, CHROs implement talent strategies that reach diverse candidate pools and ensure equitable development opportunities. With intense competition for skilled healthcare professionals in mind, CHROs develop innovative talent acquisition strategies and retention programs to attract and retain top talent, update performance management structures, and consider new models of work that may better reach business and leadership objectives. At a time when employee engagement continues to be low and burnout remains a concern, CHROs ensure their talent strategy resonates with healthcare professionals. Employee listening strategies, combined with change initiatives that provide visible improvements to healthcare professionals’ day-to-day work lives, are critical for sustaining engagement.
Moreover, CHROs need to advance and take the lead in redesigning roles and work in healthcare, which means redefining job descriptions, reassessing workflows, cross-training team members, and implementing new tools and systems to improve efficiency and quality of care. This requires a deep understanding of financial pressures, technological advancements, and workforce trends, as well as the courage to make bold decisions and drive innovation.
Culture Ambassador
Culture represents organizational “personality” that shapes the behavior of healthcare professionals throughout their organization. Although the CEO is responsible for setting the desired organizational culture, the CHRO should partner in bringing to life a culture that is engaging, promotes innovation, and delivers top clinical and business performance. For healthcare professionals, it is essential to have a supportive environment where they can see the positive impact they have on patients, their families, and communities and feel safe doing their best work. The culture either allows or hinders those experiences through high-level organizational policies and processes down to team culture, interactions, and behaviors that align (or not) with cultural values. The CHRO communicates the company’s vision and values to healthcare professionals and works with business partners, frontline managers, and clinical leaders to cascade and embed culture consistently across the organization.
Change Agent
Today’s healthcare CHROs face a variety of challenges that drive change, including mergers and acquisitions, layoffs, the implementation of new technologies, updates to business strategies and branding, as well as societal and environmental factors. Additionally, healthcare regulations are constantly evolving, which requires CHROs to stay informed and ensure compliance throughout the organization. Modern CHROs lead and champion organizational transformation initiatives while strategically addressing barriers to adoption and cultivating an environment of readiness for change among all teammates. They need to have experience in developing effective change management plans, communicating them clearly, and inspiring team members to adopt and utilize changes.
Strategic Connector
CHROs have become strategic leaders within the C-suite. They are now integral in shaping organizational strategy, particularly in areas like talent management and organizational development, and aligning talent strategies with broader organizational goals to enhance patient care and operational efficiency. With the rise of partnerships and external collaborations, CHROs must build purpose-driven connections with various institutions both within and outside of healthcare to learn best practices for more effective and efficient HR functions. This includes collaborating with educational institutions to establish talent pipelines, partnering with technology companies for digital solutions, and working with other healthcare providers for shared services. Effective communication and relationship-building skills are essential for CHROs when interfacing with a diverse range of constituents, from unions to business leaders.
Equipping Healthcare CHROs for Success
Given the dynamic nature of healthcare and the key facets of successful CHROs, several proactive and strategic recommendations are included. Drawing upon WittKieffer’s extensive industry expertise and executive search and leadership advisory work with healthcare clients, these recommendations aim to help CHROs navigate the evolving landscape, seize opportunities, and address leadership challenges effectively.
HR Functional Expert
- Stay ahead of the curve: Proactively develop future-focused approaches to HR functions that are responsive to shifts and keep pace with new human capital demands. Stay informed about the latest trends and innovations in HR functions (within and outside of healthcare) and in the healthcare market.
- Build a strong HR team: Invest in building a high-performing HR team with diverse skills and expertise. Provide your HR team members with the necessary training and development opportunities to ensure that they are equipped to meet the changing demands and novel challenges of the healthcare industry.
- Champion tech-driven transformation: Embrace digital transformation and AI integration. Stay up-to-date with the latest technological advancements and proactively integrate them into HR strategies to support more cost-effective, equitable, and innovative HR operations.
Talent Strategist
- Develop innovative talent strategies: With intense competition for skilled healthcare professionals, develop innovative talent acquisition strategies, retention programs, and learning and development opportunities to attract and retain top talent and position your organization as a talent magnet in the market.
- Prioritize succession planning: Develop and implement succession planning strategies that ensure long-term leadership continuity and sustained organizational success. Identify strategically vital roles — existing and emerging — and high-potential talent for those roles; provide them with the necessary development opportunities to prepare them for future leadership roles.
- Embrace change: Take a proactive approach to redesigning roles and work to ensure that your organization is well-positioned to meet future challenges and provide high-quality care to patients. Embrace change, stay ahead of the curve, and enhance your employer’s brand as a leader in the field to attract top talent.
Culture Ambassador
- Align culture with organizational goals: Partner with the CEO to set the desired organizational culture, ensuring that it aligns with business and talent objectives and supports the business strategy. Work with business partners, frontline managers, and clinical leaders to cascade and embed culture consistently across the organization.
- Prioritize safety: Make patient and workforce safety a core cultural value. Prioritize physical and psychological safety by implementing prevention and control standards, policies, and strategies to mitigate safety hazards.
- Lead with compassion: Foster a culture where all teammates feel recognized, appreciated, and involved. Promote a deeper understanding of health disparities within the context of clinical, social, and environmental determinants to advance empathetic and patient-centered healthcare practices across the organization.
Change Agent
- Develop a strategic communication plan: When facing significant changes, use strategic and effective communication to keep team members informed. Prepare a thoughtful communication plan that includes a clear cadence, target groups, and messaging. Make change communications more human-centric by expressing the need for the change in a way that connects teammates to the benefit of the change for the organization and themselves.
- Involve teammates in the change process: Engage team members by soliciting their input and feedback to increase buy-in and reduce resistance to change, as well as to ensure that the changes are aligned with the needs and goals of the organization. Consider nominating champions who can act as change accelerators and message multipliers.
- Address change fatigue: Prioritize the most critical changes and communicate clearly about the reasons for each change. Proactively identify legacy processes or procedures that may hinder change or create confusion around the desired behaviors and outcomes of change initiatives and focus on them. Show empathy and provide support and resources — and opportunities for rest and recovery.
Strategic Connector
- Align talent and business strategy: Understand the organization’s strategic goals and operational needs to ensure that the organization has the right people with the necessary capabilities to execute them. Help align the leadership team to bring out the best in the organization and each other.
- Build a compelling business case: To secure C-suite buy-in and resources for HR initiatives, prepare a business case that demonstrates the value of those initiatives, quantifying their impact on clinical and business performance, demonstrating their ROI, and providing a framework for measuring the success of HR initiatives and making adjustments as needed.
- Build a network of peers: To stay up-to-date on best practices, emerging trends in HR, and key leadership topics, build a network of peers or a community of practice with other HR leaders in healthcare and other industries, as well as experts in talent management, organizational development, and other relevant fields.
To address market dynamics in healthcare and growing business demands, the role of CHROs is becoming more complex and multifaceted, requiring a strategic and interconnected approach. By leveraging five key facets of successful healthcare CHROs — HR functional expert, talent strategist, culture ambassador, change agent, and strategic connector — CHROs can effectively meet their organization’s unique challenges and opportunities, ultimately driving transformation and innovation in healthcare.
Research Methodologies
All analyses were conducted in 2024 and are proprietary to WittKieffer:
- Route to the top of CHROs in healthcare: To gain deeper insights into the career paths of CHROs in healthcare, WittKieffer’s team conducted research with a focus on the top 200 health systems in the United States by annual revenue, as designated by Definitive Healthcare. For each sitting CHRO, publicly available information was collated from various sources, including organization websites, press releases, BoardEx, and LinkedIn. This information was used to construct a comprehensive dataset of career experience, industry exposure, educational background, and other relevant metrics. Subsequently, the dataset was analyzed to identify common trends and patterns in the career paths of today’s CHROs in healthcare.
- Leadership profile analysis: Drawing from the extensive experience of WittKieffer’s consultants in hundreds of executive search engagements to identify and attract CHROs in healthcare organizations, WittKieffer’s team analyzed 70+ leadership profiles of health system CHROs that were instrumental to searches conducted from 2018 to 2024. The focus of the analysis was on the evolution of the CHRO mandate, goals, and responsibilities, as well as the qualifications required.
- Route to the top of CHROs in S&P 250 companies: As a comparator group, WittKieffer focused on CHROs at S&P 250 companies to explore the career paths of CHROs across industries. In addition to demographic data and professional experience, the research included a deeper look into cross-industry moves into a current CHRO position.








